INTRODUCTION
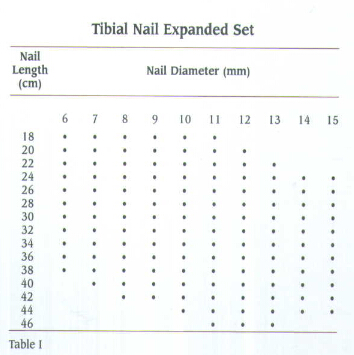
The major advantage of the tibial interlocking nail is the use of the closed technique during insertion as well as the ability to lock the nail proximally and distally to resist axial forces and shortening of the tibia. M/DN Tibial Interlocking Nails range in diameters from
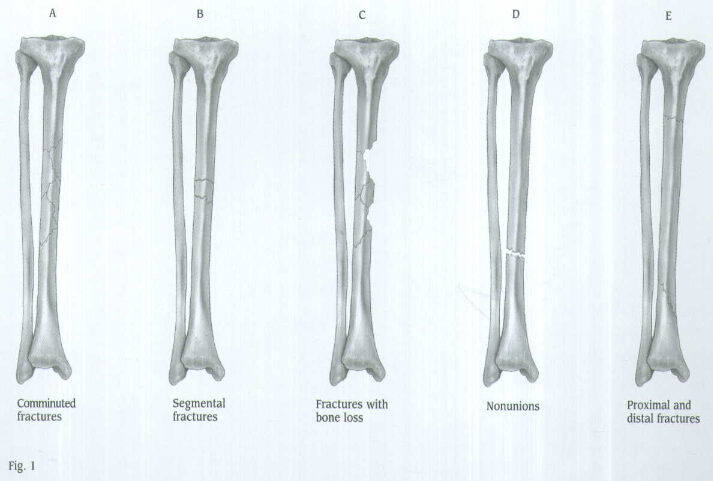
INDICATIONS(FIG.1)
The Tibial Nail is indicated for use in a variety of tibial fractures, such as:
A. Comminuted fractures
B. Segmental fractures
C. Fractures with bone loss
D. Nonunions
E. Proximal and distal fractures
PREOPERATIVE PLANNING
Proper preoperative planning is essential to success-ful interlocked nailing of the tibia. A template or Ossimeter, and an x-ray film of the unaffected extremity are necessary for determining canal size and for measuring the length of the tibia to aid in determining nail length.
Harris/Galante Bulb-tipped Guide Wires (Sounds), available in diameters from
X-rays taken at a 36-inch distance from the x-ray source result in 10-15 percent magnification of bone. The M/DN Ossimeter has both an actual size scale and one that takes into account this magnification. It should be used routinely to determine nail diameter and length.
The proper length of the nail should extend from
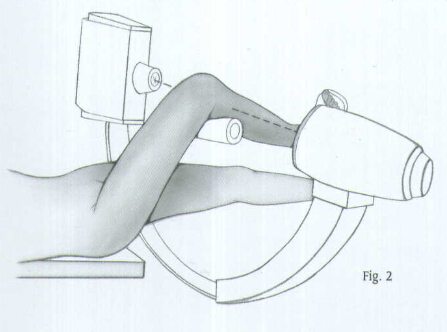
PATIENT POSITIONING AND RADIOGRAPHIC CONTROL
Place the patient in the supine position of the fracture table with the injured extremity in traction and the knee in flexion. Place the counter traction bar at the level of the distal thigh and not in the popliteal fossa (Fig.2).Place the unaffected leg in a leg holder so it is held straigth to allow easy access for the C-arm to the injured extremity. Visualize the knee as well as the shaft of the tibia using image intensification to confirm proper positioning prior to prepping and draping.
An alternative method of positioning is to place a radiolucent frame under the knee.
Another alternative is to place the patient on a radiolucent table, using a distractor for fracture reduction.
REDUCTION
It is important to reduce the fracture before beginning the surgical procedure.
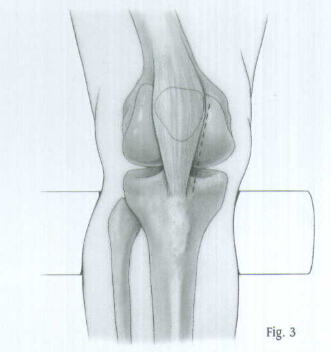
INCISION AND EXPOSURE
Make a longitudinal incision along the medial border of the patellar ligament extending from the joint line to the inferior pole of the patella (Fig.3). Carry the dissection medially to the patellar tendon down to the bone. Place a Blunt Retractor beneath the patellar ligament and retract the ligament laterally to expose the proximal tibia.
CREATING THE ENTRY PORTAL
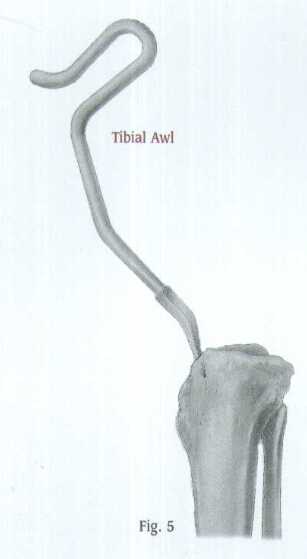
Place the Tibal Awl medial to the patellar tendon and at the top of the tibia (Fig.4). Fox proximal fractures, either split the patellar tendon or position the wal lateral to the tendon to prevent angulation at the fracture site. Check the position with A/P and lateral views. When the correct position is achieved, rotate the awl to create an entry portal for the Bulb-tipped Guide Wire (Fig.5).

GUIDE WIRE PLACEMENT AND REAMING
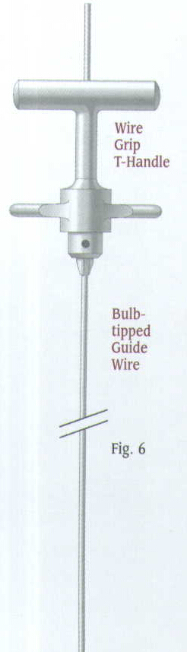
Attach the

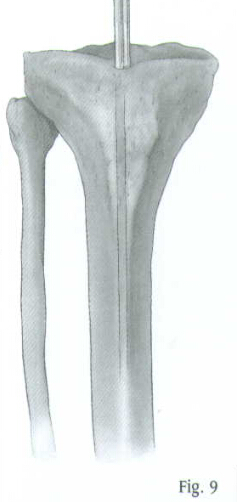
Determine the proper nail length by placing a second guide wire of equal length on the proximal tibia. The length or the wire that is not overlapping is the correct nail length required (Fig.9). The
Another way to measure the length is to use the C-arm to position the 0 mark on the metal ruler at the distal tibial epiphyseal scar. Then read the correct length at the proximal tibia directly off the metal ruler.
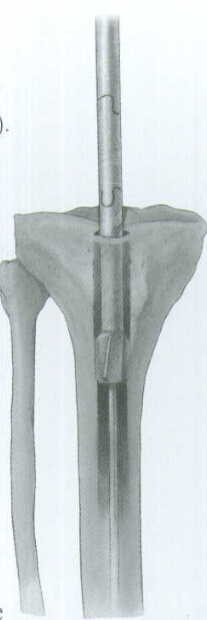
Place the Skin Protector in the wound. Then place an intramedullary reamer over the guide wire and ream the tibial canal in 1 millimeter increments until contact is made with the cortical wall. Continue to ream in 1/2 millimeter increments up to 1 millimeter greater than the selected nail diameter (Fig.10). During reaming, monitor the lateral view on the image intensifier to prevent excess reaming of the posterior cortex.
The proximal diameter of the
Remove the Bulb-tipped Guide Wire and insert the Smooth Guide Wire (Fig.11). Note:

NAIL INSERTION
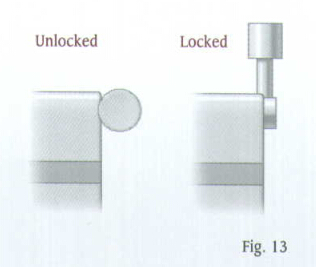
Attach the selected nail to the Tibial Proximal Guide. A keyway in the proximal end of the nail will help ensure proper alignment. Be sure the arrow on the proximal guide is pointing to the appropriate ''Left'' or ''Right'' indication (Fig.12). Lift and turn the ratchet lever 90 degrees to open the ratchet mechanism of the Proximal Guide (Fig.13).

Insert the locking Bolt through the barrel of the guide (Fig.14). Lift and turn the ratchet lever 90 degrees to close the ratchet mechanism, and use the Pin Wrench to tighten the Locking Bolt into the proximal end of the nail. The ratchet mechanism will prevent the bolt from loosening during insertion of the nail.
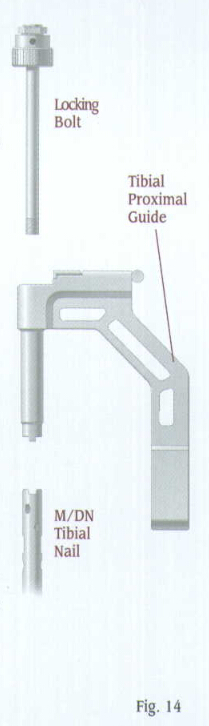
Note: If the ratchet mechanism of the Tibial Proximal Guide does not operate freely, it may be necessary to disassemble, clean, and reassemble the mechanism. If the ratchet mechanism becomes inoperative, it may be removed. The assembly will still function; however, the Locking Bolt may loosen during the procedure.
Verify proper alignment by inserting the
Screw the Threaded Driver or Slaphammer into position on the Locking Bolt. Insert the nail over the Smooth Guide Wire and into the tibia. Begin seating the nail using bentle impaction with the mallet(Fig.16). The nail must advance with each blow of the mallet. If it does not, remove the nail and ream again. While impacting the nail, use the Tibial Proximal Guide to maintain the proper rotation.
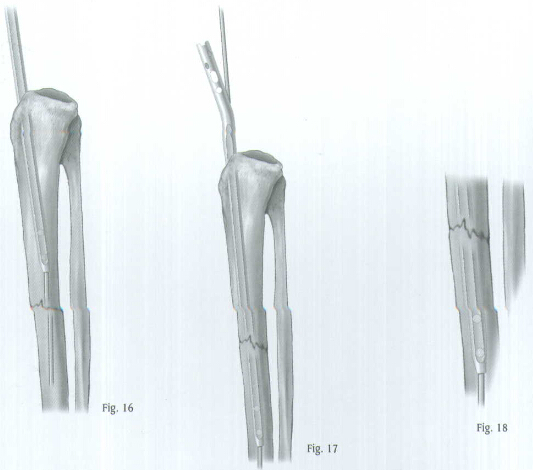
Be careful when crossing the fracture site. Visualize the fracture in two planes with image intensification to assure proper passage of the nail into the distal fragment (Fig.17). The conical tip and the bevel of the nail will help guide it off the posterior cortex and maintain its position in the center of the canal (Fig.18). Reduce the force of impaction as the proximal end of the nail approaches the tibial tubercle.
Prior to inserting the nail past the guide wire exit hole, REMOVE THE GUIDE WIRE so it does not get trapped in the bone. Finish seating the nail after the guide wire is removed.
PROXIMAL LOCKING
The M/DN Tibial Nail has four proximal locking holes. The two superior holes are angled for fixation in very proximal fracture situations.
The middle hole is a mediolateral dynamic slot to help achieve dynamization. The most inferior mediolateral hole is for static locking. If static locking is preferred, but there is a potential need for later dynamization, insert screws in both mediolateral locking holes. The locking screw in the static hole can then be removed to achieve later dynamization.
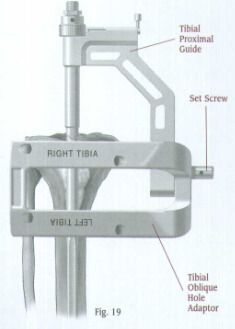
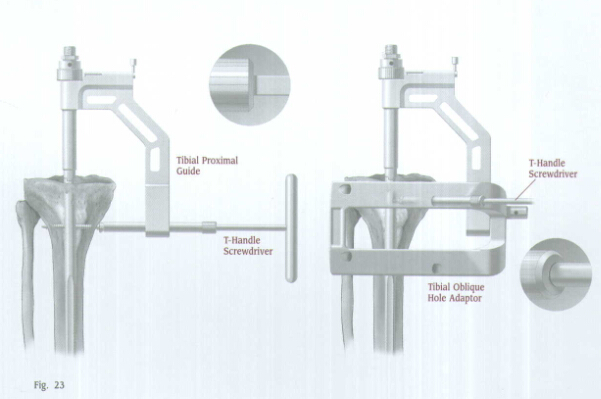
If oblique fixation is desired, attach the Tibial Oblique Hole Adaptor to the Tibial Proximal Guide (Fig. 19) so the appropriate''Right''or''Left''indication is up. Secure the adaptor with a set screw, and tighten the screw with the Pin Wrench.
The adaptor has four holes. Two holes are for the left tibia, and two holes are for the right tibia. Use the two top holes. One hole is for anterolateral to posteromedial screw insertion. The other hole is for anteromedial to posterolateral screw insertion.
Tibial Proximal Guide
Set Screw
Tibial Oblique Hole Adaptor
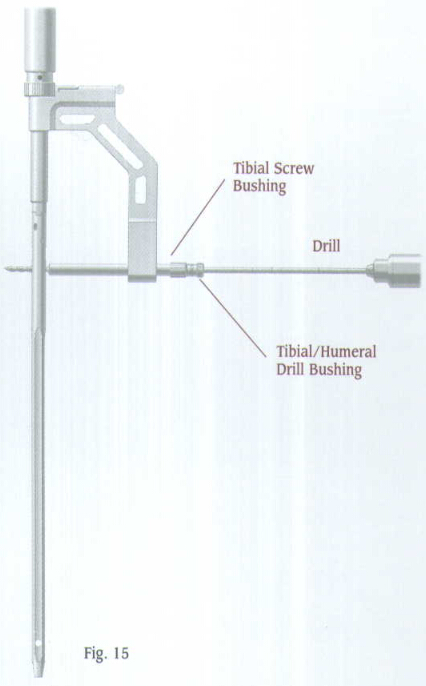
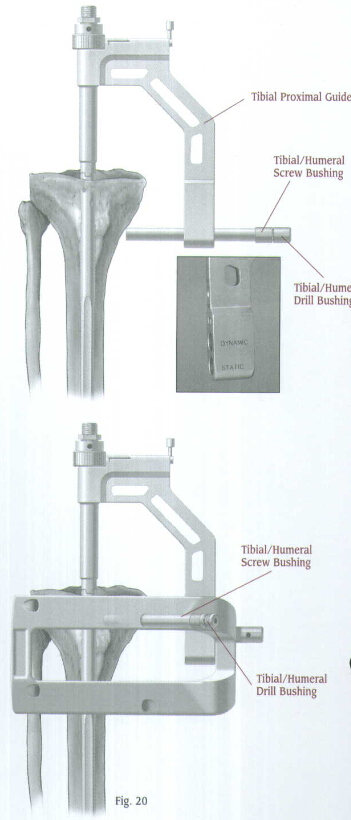
Insert the
Make a small stab wound, then advance the nested bushings through the incision until they contact the medial aspect of the bone (Fig.20). Insert the
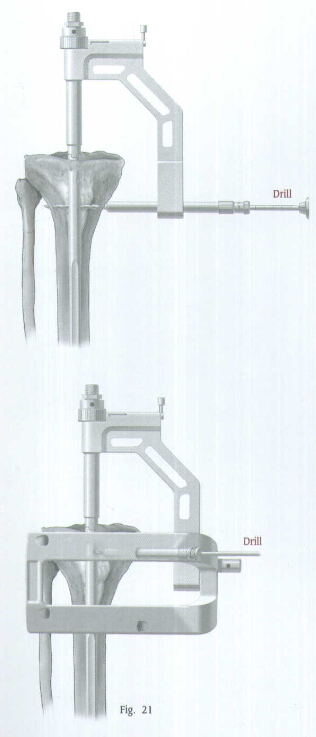
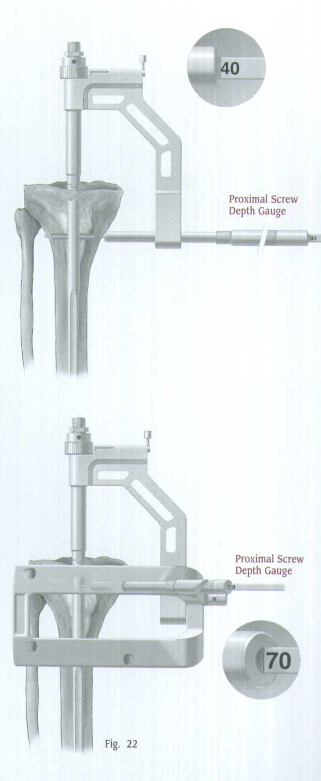
Drill through both cortices (Fig.21). The drill is calibrated to measure the hole depth and determine the appropriate screw length. If desired, the Proximal Screw Depth Gauge can also be used to determine the screw length (Fig.22). Remove the drill and drill bushing.
The 4.2 or
Use the T-Handle Screwdriver to insert the appropriate length 4.2 or
If a second proximal screw will be used, repeat the procedure for the second screw.
Take A/P and lateral C-arm views to check for correct positioning. Disengage the ratchet mechanism, then loosen and remove the Locking Bolt and Tibial Proximal Guide.
END CAP PLACEMENT
Insert an M/DN End Cap of the appropriate length (
DISTAL LOCKING
Technique for Using the Free-Hand Targeting Device
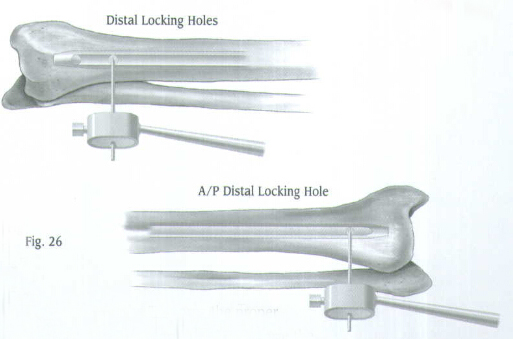
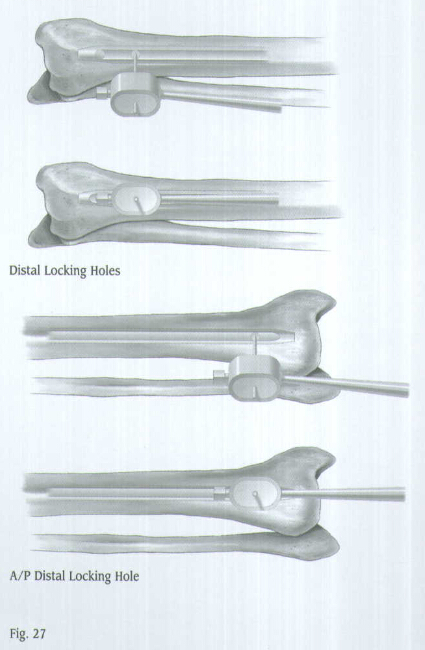
The distal locking screws are inserted with a free-hand technique using the Free-Hand Targeting Device. The M/DN Tibial Nail has three distal holes. Two are located for locking in the mediolateral plane, and one is located between the mediolateral holes for locking in the anteroposterior plane.
Note:
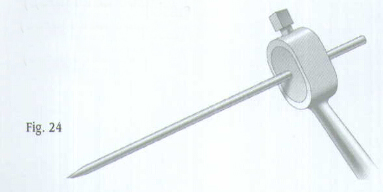
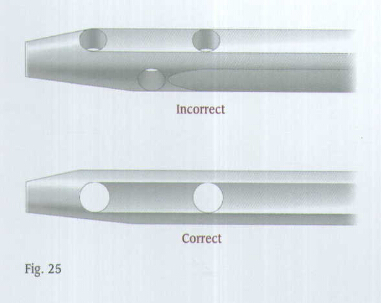
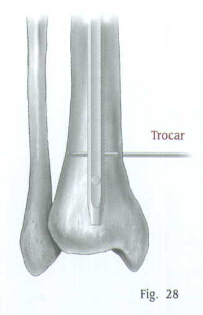
Insert the appropriate size Trocar into the Targeting Device and finger tighten (Fig.24). It is very important to properly place the C-arm. Position the C-arm so the locking hole of the nail appears perfectly round on the monitor (Fig.25).
Make a
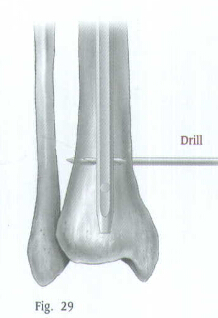
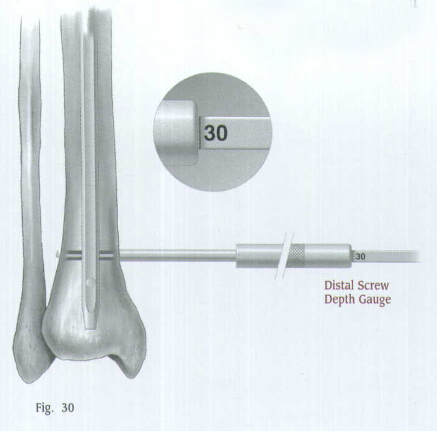
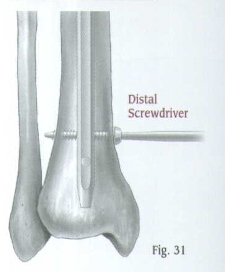
Use the Distal Screwdriver to insert the screw through the hole (Fig.31).
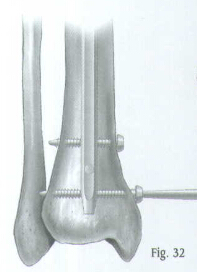
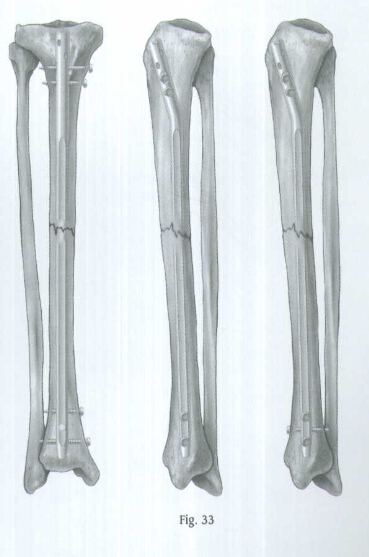
Insert the second and third distal locking screws in the same manner (Fig.32). Check the position of all screws with the C-arm in the A/P and lateral planes (Fig.33).
Bushings are available that can be used with the Free Hand Targeting Device. A separate radiolucent Bushing Insert is available to accommodate the bushings.
CLOSURE AND POSTOPERATIVE CARE
After irrigating the wounds, close the proximal wound in layers. Then apply a soft compression dressing.
A short leg splint is used until pain and sweling are decreased. Then early range-of-motion exercises of the knee and ankle are encouraged. Allow toe-touch weight bearing to progress to full weight bearing as fracture callus increases on x-ray films, usually six to eight weeks.
EXTRACTION
Should extraction of the nail become necessary, attach the Threaded Extraction Adaptor